
Preventing reinjury: How neuroplasticity and biomechanics are changing injury recovery
The phrase 'mind over matter' is getting a whole new meaning as OHIO researcher Dustin Grooms and his team work to discover ways to prevent reinjury by looking at the way the brain plays a role in recovery.
Samantha Pelham | August 26, 2024
Share:
It's disheartening to get injured, and even more so to invest time and effort into rehabilitation only to find yourself in the same or worse condition. However, researchers at the Ohio Musculoskeletal and Neurological Institute (OMNI) are exploring innovative solutions to reduce reinjury risk, and the key to success might lie in understanding the brain's role in recovery.
Dustin Grooms, a professor of Physical Therapy in Ohio University’s College of Health Sciences and Professions, is helping lead advances at the intersection of biomechanics and neuroplasticity. Grooms leads a dynamic research team focused on how the brain adapts following orthopedic injuries, with the goal of preventing reinjury and allowing people to live a long, happy and easy life.
"We're not just treating injuries; we're unraveling the mysteries of how our brains adapt and heal," Grooms said. "It's a journey of discovery with profound implications for athletes, military personnel and beyond. Our approach isn't just about rehabilitation—it's about optimizing performance and longevity.”

Ohio University researcher Dustin Grooms leads groundbreaking advances in biomechanics and neuroplasticity.
His early experiences in athletic rehabilitation revealed that athletes often struggled with reinjury and incomplete recovery despite advanced treatments. This led him to pursue a Ph.D. in neuroscience & biomechanics to explore how neuroplasticity can improve rehabilitation outcomes.
“You start out in this field with the hope that everyone you treat will get better, but you get into the real world and realize there is a lot more we need to understand and gray area in our work that surpasses just rehabilitating a single injury,” Grooms explained. “I witnessed firsthand the challenges athletes faced in fully recovering. Even with the latest treatments, many experienced reinjury or couldn’t return to their previous level of performance. This drove me to seek a solution that would not only benefit athletes but also ensure that everyone could achieve long-term, healthy recovery."
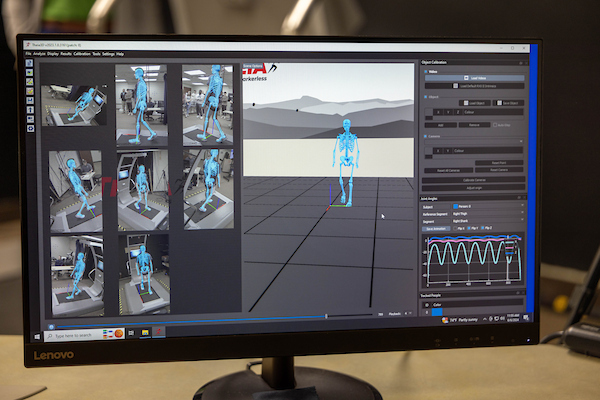
Traditionally, orthopedic injuries were viewed as purely affecting the bodies structure, but Grooms’ research has shown that the brain undergoes significant changes to compensate for lost proprioception—the body’s sense of joint position. Using advanced technologies like motion capture, functional MRI (fMRI), virtual reality (VR), and augmented reality (AR), Grooms and his team examine how the brain processes and adapts to these injuries. VR and AR are used to simulate real-world scenarios, enhancing proprioception and reducing the risk of reinjury, specifically among athletes and military personnel. This innovative approach allows for improved assessment and neurological control of movements, challenging conventional rehabilitation methods.

Grooms’ recent collaborations with institutions such as the Cincinnati Children's Hospital and Emory University focus on using AR to enhance neuro-control of knee movements in pediatric athletes, particularly to prevent ACL tears which is more prevalent in adolescent females. Additionally, projects funded by the National Institute of Health (NIH) and the Department of Defense include exploring novel rehabilitation strategies using strobe glasses to optimize brain function. These initiatives aim to improve not only injury recovery but also overall performance and longevity.
“A lot of times when we see athletes or members of the military get reinjured it’s because their brains were not ready to go back into their fields,” Grooms explained. “We are using VR to occupy vision so you can’t see your joints, allowing your brain to get comfortable with proprioception again and strengthen it.”
The intersection of sports and military training presents unique challenges where high visual attention is critical. Complications arise when individuals return to their activities prematurely, believing themselves ready but lacking neurological readiness. To address this, VR is employed to occupy visual perception, allowing individuals to focus on proprioception without relying on sight. By simulating various scenarios, from tactical operations to everyday movements, VR helps assess and improve how individuals respond to stimuli. It serves not only as a standardized testing tool but also as a training aid, mimicking real-world conditions to enhance proprioceptive skills crucial for injury prevention and performance optimization. This approach ensures that athletes and military personnel can regain confidence in their movements, reducing the risk of reinjury by aligning brain and body functions effectively.
With the Department of Defense grant, Grooms and his team will track brain changes, determining optimal interventions during therapy and test innovative ideas, including the use of strobe glasses to enhance proprioception. According to Grooms, athletes like Stephen Curry have utilized these glasses to improve visual processing, a technique now integrated with cutting-edge rehabilitation innovations designed to optimize movement control.
Among the researchers working on this project also include OHIO Ph.D. students HoWon Kim and Amber Schnittjer, as well as BME masters student Zoe Miller and post-doctoral fellow Justin Rush, who will explore sensory prediction errors contributing to injuries, using advanced biomechanics equipment like markerless motion capture and a treadmill that can induce stumbles in a safe manner to quantify the detection and correction of these motor errors. Dr. Janet Simon and Dr. Melissa Anderson are also helping co-direct many of the projects alongside Grooms, with Byrnadeen Farraye acting as project manager\research associate, managing many of the projects.

“OMNI is truly a collaborative unit both between the two centers that make up the institute, and the various levels of expertise and areas within it. We all have the common goal of finding ways for people to age more gracefully, with higher function and less injury risk,” Grooms said. “Although the two centers focus on different areas, they are also correlated. Injuries that occur in young patients impact how they age and the rate in which their bodies age, with injury accelerating the aging process.”
With plans to integrate their research and work into the new Heritage Translational Research facility, Grooms envisions expanding their capabilities in brain imaging and biomechanics. Grooms is hopeful to find a way for OHIO to acquire an advanced version of neuroimaging called Magnetoencephalography or MEG that is set to replace research MRI in the near future to continue pushing the boundaries of what's possible in understanding human movement and enhancing rehabilitation outcomes.
